The Herniated 'Slipped' Disc and Lower Back Pain
Anatomy, Risk Factors, PAthology & Management
Fortunately for us, the notion of a herniated intervertebral disc to suddenly 'slip out of its place' is physically impossible. Discs found in between vertebrae of the spine are firmly attached to these structures, however, they can wear, split or herniate (bulge outwards).
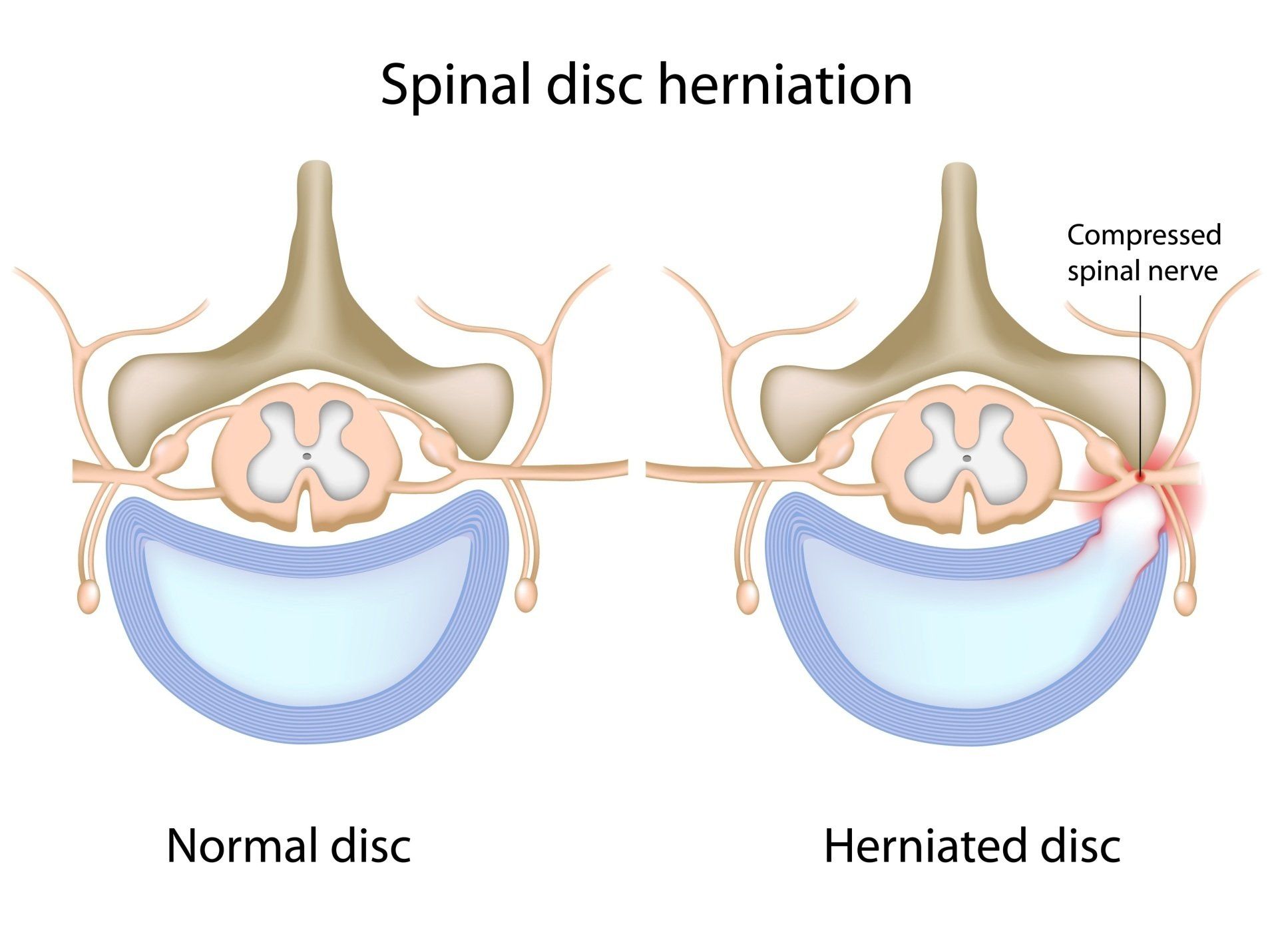
The term herniation is a term used to describe the displacement of
focalised intervertebral disc material which is beyond the limits of the disc's
space (11, 16). The classification of the herniated disc depends on either the
annulus fibrosus (AF), the disc's outer and tougher covering. Or, the nucleus
pulposus (the jelly like center of the disc) (18).
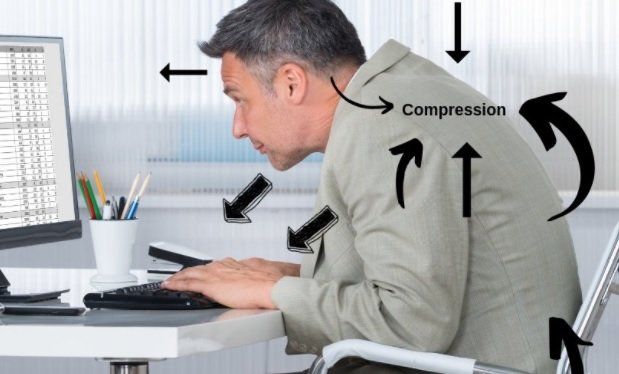
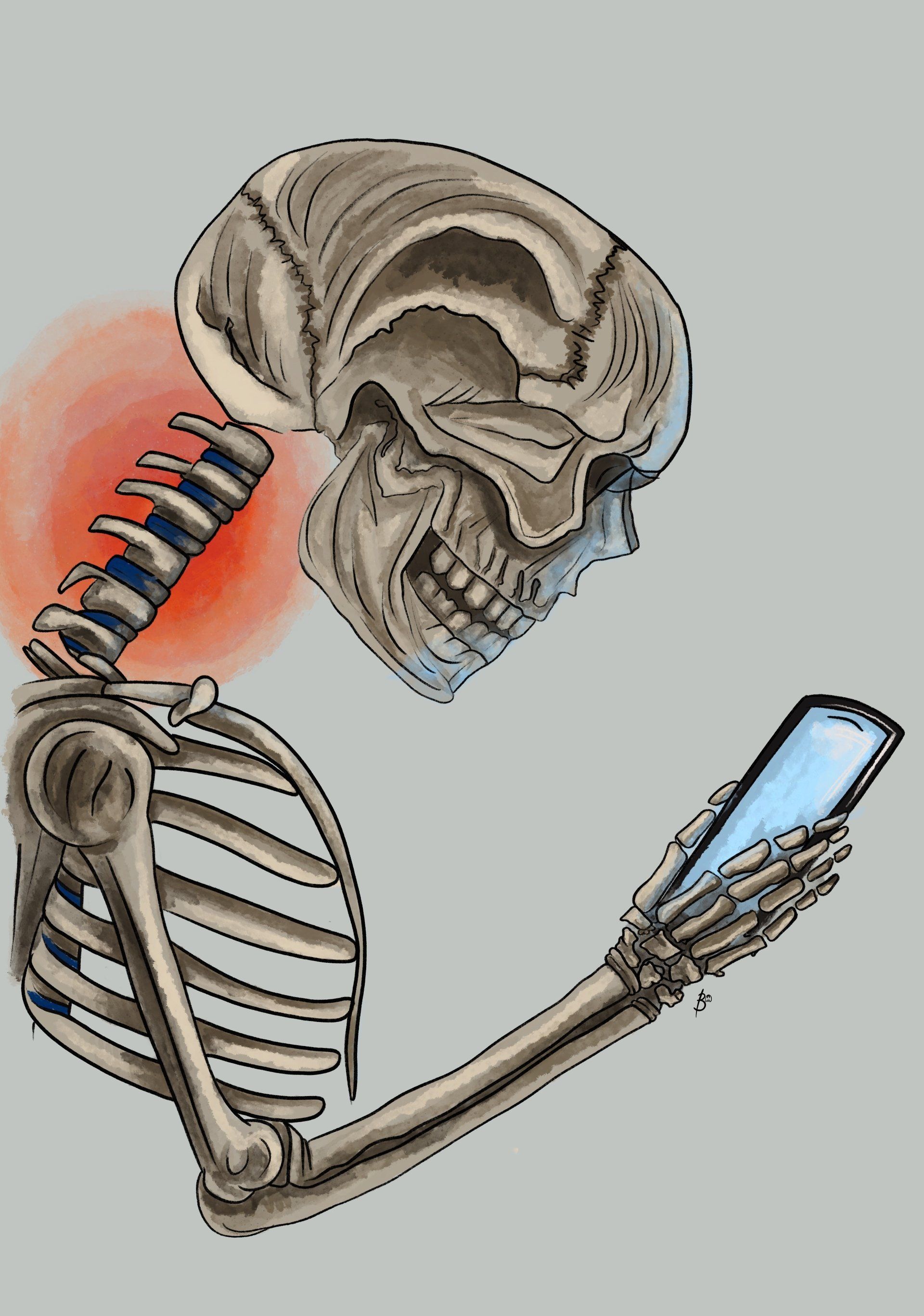
Disc herniations can be as a result of of a sudden injury to the structure such
as a trauma, progressive degenerative changes or from repetitive stress from
certain activities at work or during exercise (8, 18).
Biomechanical studies have
mainly found that injury to a disc rarely occurs via axial compression
alone (or spinal compression which causes shortening along the spine
curvature) (7, 18). Instead, spine shrinkage and the development of disc
herniations are more commonly caused from the repetitive motions of
forward spinal bending (flexion) and rotation (torsion) (7, 23).
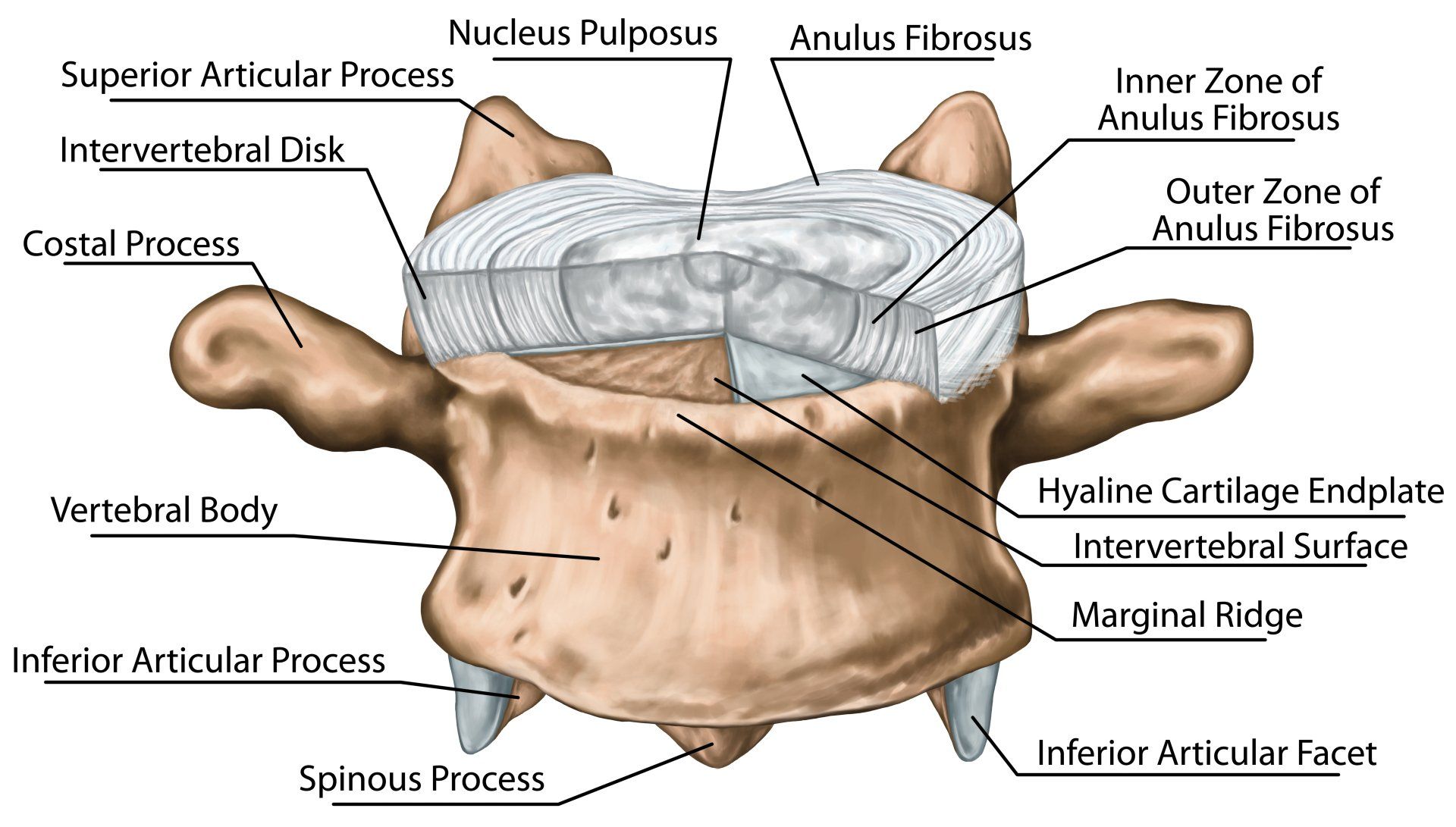
Anatomy of the Intervertebral Disc
The intervertebral disc (IVD) is the largest avascular structure in the body and serves to allow movement between adjacent vertebral bodies, absorb shock and transmit loads through the vertebral column (5, 9). The IVD are mainly composed of three parts:
- Annulus fibrosis
- Cartilaginous vertebral endplate
- Nucleus pulposus
Annulus Fibrosus (AF)
The AF is the primary load-bearing component of the IVD and is composed of collagen fibers which are tightly arranged in 10-20 sheets of lamellae (2, 3). These are arranged and positioned in onion like rings around the central nucleus pulposus and the alternating alignment of fibers within the layers account for its strength and its ability to withstand the forces applied to the disc in all directions (2, 11). The directions of the layers of the annulus fibrosus alternate which adds to the strength of the annulus fibrosus. The posterolateral aspect of the annulus fibrosus has a greater content of vertically oriented fibers which weakens the disc tissue and explains why most annular fissures occur at this particular region of a disc (17).
The AF of the lumbar spine IVDs are at their thinnest posteriorly by only having half the thickness of the anterior and lateral aspects of the annulus as there are fewer, finer and more tightly packed collagen fibers (lamellae) (2, 11). This makes the area of the AF more susceptible to injury at the lumbar intervertebral disc, especially if torsional (rotational) forces are applied.
Vertebral Endplates (EPs)
EPs are cartilaginous structures that are stongly attached to the
intervertebral disc (IVD) via the annulus fibrosus but weakly attached to the
vertebral bodies (2, 11). The endplates are situated superiorly and inferiorly
in every disc and cover the whole length of the nucleus pulposus, but do not
cover the entire extent of the anulus fibosus (2). Interestingly, the endplates are strongly bound to the intervertebral disc, but, are however weakly attached to the vertebral bodies and therefore possible for the disc to tear away from the vertebral body during spinal trauma (2).
Nucleus Pulpsoes
Is an oval shaped hydrated gelatinous material contained within a ring of collagen fibres and contains mostly type II collagen which is elastic in nature and usually found in tissues that are exposed to pressure (2, 11).
The Herniated Disc; Pathology & Risk Factors
Disc
herniation can occur in any disc within the spine but the majority of disc
herniations occur within the lumbar spine, particulalry L4-L5 or L5-S1 (15).
Lumbar disc herniation is the most common spine disorder requiring surgical
intervention and it has been estimated that approximately 5–15% of patients
with lower back pain suffer from lumbar disc herniation (8). The second
most common site is the cervical region (C5-C6 or C6-C7) (15). Disc herniations
can occur at any age, but are mainly known to be experienced between the 4th
and 5th decades of life (20).
There are various personal and occupational risk factors for sciatica and
prolapse discs which include (3):
- Smoking
- Obesity
- Age
- Height
- Mental Stress
- Exposure to vibration from vehicles
Types of Injury To the Intervertebral Disc
Annular
Disc Tear
This is when a tear or fisure occurs within one or more layers of the annulus
fibrosus and most are asymptomatic. Symptomatic annular tears or fissures
without disc herniation are treated with NSAIDs and physical therapy (17).
Thus, even if a disc prolapse or annular tear is discovered via medical imaging
(e.g. MRI), pain is NOT necessarily experienced.
Pain from an annular tear might either be acute if the tear occurs suddenly or more chronic if there is a slower development of the annular fissure. If an annular fissure or tear is symptomatic, it may cause one of two findings:
1. Localised pains that are secondary to an annular tear might might be worse during certain movements which can stress or irritate the focal annular tear. In such cases, there is no radicular nerve involvement, and the physical exam may be unrevealing.
2. Radicular symptoms secondary to irritation of the passing nerve root. In some cases, an annular tear can irritate the traversing nerve and cause radiculopathy (due to be explained in another blog post). If the annular fissure or tear is deep enough, disc material can herniate and irritate or compress neighbouring nerves or the spinal cord which can cause radicular symptoms including pain, paresthesia, and/or weakness depending on the extent of nerve irritation (17).
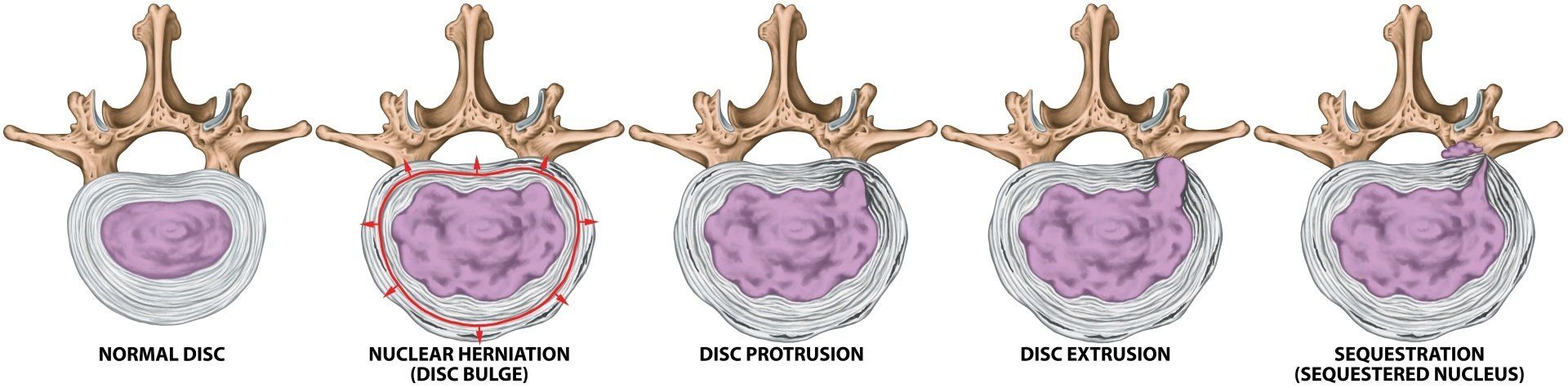
According to Ma (2015), the pathological classification of lumbar disc protrusion is controversial and the study describes four different types of lumbar disc protrusion. To keep matters simple, four problems of the intervertebral disc resulting from injury have been listed and briefly explained below:
Disc Protrusion
In a protruded disc, the disc bulges posteriorly without rupture or tearing of the annulus fibrosus (13).
Prolapsed Disc
The outermost fibers of the annulus fibrosus (AF) contain the nuceleus Pulposus (13).
Disc Extrusion
The annulus fibrosus (AF) is perforated and part of the nucleus pulposus (NP) moves into the epidural space (13).
Sequestration
When a formation of discal fragments from the annulus fibrosus (AF) and nucleus pulposus (NP) is no longer connected to the disc (13).
Disc extrusion and sequestration are most likely to cause radicular symptoms. Disc sequestration does sound and appear alarming compared to the other types listed above and one might think that surgical intervention would be the only way forward for recovery. But, it has been known for patients to recover completely from this condition and be reversible after nonsurgical conservative management.
The study by Orief (2012) revised six patient case studies who had experienced and been diagnosed with a symptomatic sequestrated disc levels L4-5 in three cases, L5-S1 in two cases, and C5-6 in one case. All six patients experienced associated acute radicular pain due to sequestrated intervertebral disc herniation and refused surgery as they were worried about complications. All six patients received conservative treatment that consisted of oral anti-inflammatory drugs, analgesics, muscle relaxants and physical therapy. Their radicular painsdiminished and recovered within 3 to 6 weeks and resorption of the sequestrated intervertebral disc herniation was seen in their follow-up MRI scans after 4 to 9 months (16).
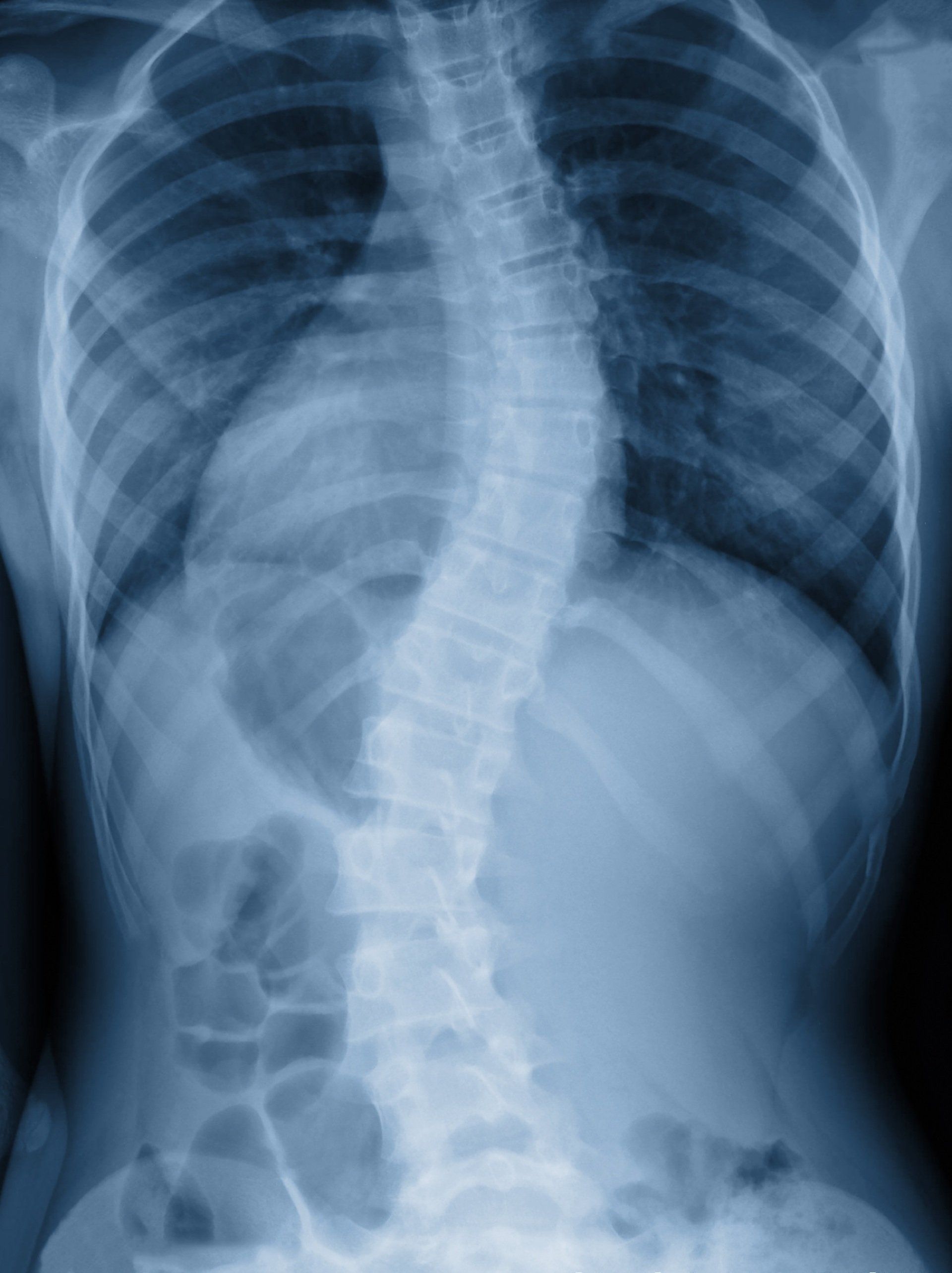
Diagnosing a Herniated Disc
The diagnostic accuracy of taking a case history and performing a physical examination is still insufficient. Diagnostic imaging in patients is often used to assess nerve root compression caused by disc aviation or spinal stenosis and cauda equina syndrome. Imaging is also used to identify the affected disc level before surgery or medical intervention (6,7).
Magnetic resonance imaging (MRI), computed tomography (CT), x-ray and myelography are used as a form of diagnostic imaging.
XRay is the most commonly used form of imaging technique due to its lower cost and ready availability (6).
Magnetic resonance imaging (MRI) Scans are mostly used out of all forms of imaging for suspected lumbar spine pathologies.
Computer Tomography (CT Scan) is less costly than the MRI, its testing time is shorter and the availability of CT scanners is larger in hospital settings but has the drawback of exposure to ionising radiation (6). Myelography involves the injection of contrast medium of the lumbar spine followed by x-ray CT or MRI imaging.
Recovery & Treatment
Studies
suggest that patients who have suffered a lumbar disc herniation tend to
improve in 6 weeks and conservative therapy is recommended during this time if
major neurological deficit is absent (4). Overall, initial management includes rest as indicated, physical
therapy and appropriate use of pain medication.
Recovery
Individuals who have motor deficits within a single nerve root as a result of disc herniation which lead to symptoms such as weakness during dorsiflexion of the foot, or foot drop tend to improve over time (4). Studies have shown that 81% of patients with initial muscular paresis usually recover without surgery after a year and sensory deficits may be more persistent with a recovery rate of 50% after one year (4). MRI scans show shrinkage of herniated disks over time and up to 76% partially or completely resolve by one year (4).
Recurrence Post Herniation
Recurrences of pain are common, a study conducted Suri et al.,
(2012) found that the recurrence of lower extremity radicular pain after non surgical treatment of acute lumbar disc herniation was quite a common phenomenon by reoccurring in 25% of participants over a one year duration after the resolution of leg pain (19).
Spinal Manipulation
According Deyo et al., (2016), studies have shown that patients who participated in supervised exercise had greater short-term pain relief than patients who received counselling alone, however, a reduction in pain reported to be small (4).
A study for chiropractic manipulation for subacute or chronic “back-related leg pain” showed that manipulation was more effective than home exercises with respect to pain relief at 12 weeks but not at 1 year (4).
Another study found that patients with acute sciatica and diagnosed with confirmed disk protrusion via MRI scans showed that the number of patients who underwent chiropractic manipulation benefited more than other individuals who underwent sham manipulation after 6 months of receiving treatment (55% vs. 20%) (4).
It has also been observed that skilled manual therapists who utilise mobilisation and manipulation above and below the affected spinal segment(s) and address the pelvis, or restrictions in the lower extremity, may decrease the amount of mechanical stress placed on the herniated disc(s) (17).
Surgery
Clinical trials have consistently shown faster relief of pain with surgery than with conservative physical therapy treatment. Most clinical trials show, however, that there is no significant advantage of surgery over conservative treatment with respect to relief of sciatica at 1 to 4 years follow-up (4).
Lifestyle
Data from epidemiologic studies and biomechanical models suggest that lifestyle modifications such as smoking cessation, weight loss, and regular exercise may prevent sciatica or help to reduce its recurrence (4).
References References
1.) Amin, R. M., Andrade, N. S., Neuman, B. J. (2017) Lumbar Disc Herniation, Springer, CrossMark; 10: 507-516.
2.) Bogduk, N. (2005) Clinical Anatomy of the Lumbar Spine and Sacrum: 4th Ed., Elevier, Churchill Livingstone.
3.)Carragee, E.J., Han, M. Y., Suen, P. W., Kim, D. (2003) Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am; 85: 102–108.
4.) Deyo, R. A., Mirza, S. K. (2016) Herniated Lumbar Intervertebral Disk, The New England Journal of Medicine, Clinical Practice , 374; 18: 1763-1772.
5.) Fardon, D. F., Milette, P. C. (2001) Nomenclature and Classification of Lumbar Disc Pathology Recommendations of the Combined Task Forces of the North American Spine Society, Society of Spine Radiology, and American Society of Neuroradiology, SPINE, 26; 5: E93-E119 .
6.) Frost, L. R., Brown, S. H. M. (2016) Muscle Activation Timing and Balance Response in Chronic Lower Back Pain Patients with Associated Radiculopathy, Clinical Biomechanics, Science Direct; 30: 124-130.
7.) Janardhana, A. P., Rao, S., Kamath, A. (2010) Correlation Between Clinical Features and Magnetic Resonance Imaging Findings in Lumbar Disc Prolapse, Indian Journal of Orthopedics, 44; 3: 263-269.
8.) Kadow, T., Sowa, G., Kang, J. D. (2015) Molecular Basis of Intervertebral Disc Degeneration and Herniations: What Are the Important Translational Questions? Clinical Orthopaedics and Related Research, CrossMark, Springer; 473: 1903-1912.
9.) Kim, J-H., van Rijn, R. M., van Tulder, M. W., Koes, B. W., de Boer, M. R., Ginai, A. Z., Ostelo, R. W. G. J., van der Windt, D. A. M. W., Verhagen, A. P. (2018) Diagnostic Accuracy of Diagnostic Imaging for Lumbar Disc Herniation in Adults With Low Back Pain or Sciatica is Unknown; A Systematic Review, BMC, Chiropractic & Manual Therapies, 26: 37.
10.) Koes, B.W., van Tulder, M. W., Peul, W. C. (2007) Diagnosis and Treatment of Sciatica, BMJ,
11.) Kuwahara, W., Deie, M., Fujita, N., Tanaka, N., Nakanishi,K., Sunagawa, T., Asaeda, M., Nakamura, H., Kono, Y., Ochi, M. (2016) Characteristics of Thoracic and Lumbar Movements During Gait in Lumbar Spinal Stenosis Patients Before and After Decompression Surgery, Clinical Biomechanics, 40; 45-61.
12.) Lundon, K., Bolton, K. (2001) Structure and Function of the Lumbar Intervertebral Disk in Health, Aging, and Pathologic Conditions, Journal of Orthopaedic & Sports Physical Therapy, 31; 6: 291-306.
13.) Ma, X-L. (2015) A New Pathological Classification of Lumbar Disc Protrusion and Its Clinical Significance, Orthopedics Course, 7; 1: 1-12.
14.) Magee, D. J. (2002) Orthopedic Physical Assessment 4th Ed., Saunders, Elsevier Science.
15.) Merskey, H., Bogduk, N. (1994) Classification of Chronic Pain Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms [2nd Ed.] Seattle, IASP Press.
16.) Moore, K. L., Agur, A. M. R. (2007) Essential clinical anatomy
(3rd ed.). Baltimore, MD: Lippincott Williams & Wilkins.
17.) Orief, T., O, Y., Attia, W., Almusrea, K. (2012) Spontaneous Resorption of Sequestrated Intervertebral Disc Herniation, 77; 1: 146-152.
18.) Schoenfeld, A. J., Weiner, B. K. (2010) Treatment of Lumbar Disc Herniation: Evidence-Based Practice,International Journal of General Medicine, Dove Medical Press; 3: 209-214.
19.) Suri, P., Rainville, J., Hunter, D. J., Li, L.,
Katz, J. N. (2012) Recurrence of Radicular Pain or Back Pain After Nonsurgical Treatment of Symptomatic Lumbar Disk Herniation.
Arch Phys Med Rehabil; 93: 690-5.
20.) Tenny, S., Gillis, C. C. (2019) Annular Disc Tear, University of Nebraska Medical Center, StatPearls Publishing LLC.
21.) Vangelder, L. H., Hoogenboom, B. J., Vaughn, D. W. (2013) A Phased Rehabilitation Protocol For Athletes With Lumbar IVD Herniation, IJSPT, 8; 4: 482-516.
22.) Vialle, L. R., Vialle, E. N., Henao, J. E. S., Giraldo, G. (2010) Lumbar Disc Herniation, 45; 1: 17-22.
23.) Wankhade, U. G., Umashankar, M. K., Reddy, J. (2016) Functional Outcome of Lumbar Discectomy by Fenestration Technique in Lumbar Disc Prolapse – Retunr to Work and Relief of Pain, Journal of Clinical and Diagnosis Research, 10; 3: 09-13.
24.) Waturau, K., Deie, M., Fujita, N., Tanaka, N., Nakanishi, K., Sunagawa, T., Asaeda, M., Nakamura, H., Kono, Y., Ochi, M. (2016) Characterstics of Thoracic and Lumbar Movements During Gait In Lumbar Spinal Stenosis Patients Before and After Decompression Surgery, Clinical Biomechanics, Elseiver, 40:45-51.
25.) Wisleder, D., Smith, M. B., Mosher, T. J., Zatsiorsky, V. (2001) Lumbar spine mechanical response to axial compression load in vivo. Spine, 15, 26;18: E403-9.